Cancer immunotherapy — treatments that harness the body’s immune system to fight cancer — has been gaining traction in recent years as a new approach to treating the disease.
But one of its major drawbacks is its variability: For some cancer patients, the drugs have led to remarkable remissions with few side effects. Others have tried them only to find little benefit and a lot of discomfort.
It’s something researchers have been trying to understand, exploring whether there are other drugs that could be used to boost the response in some people, or if genetics could be playing an underlying role in making it more effective in others.
And they may finally be onto something. A team of researchers has recently discovered a link between people’s responses to immunotherapy treatments and the microbes that live in their gut. Having a more diverse gut microbiome, they found, is linked to a better response.
The research, which will be presented at an upcoming medical conference, is the first study to make this link in people. Previous studies have however found similar results in mice.
The study
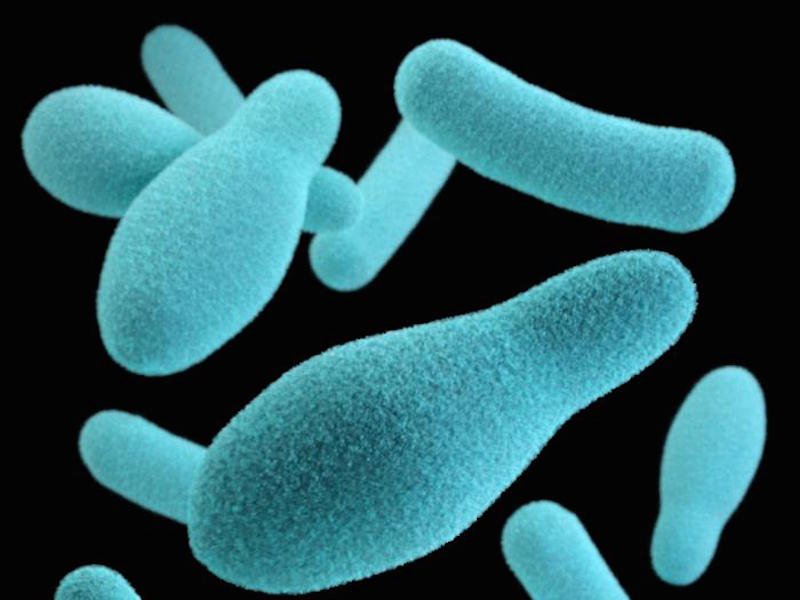
The team of researchers at the University of Texas MD Anderson Cancer Center took oral and fecal samples of bacteria from 233 patients with advanced melanoma, a type of skin cancer. For advanced stages of melanoma, the number of people still alive after two years was about 35%, compared to 29.7% over the same time for those taking chemotherapy.
Of that group, 43 patients had contributed fecal samples and were on anti-PD-1 therapy — a type of cancer immunotherapy that involves what are called checkpoint inhibitors. Among that group, 30 responded to the treatment and 13 didn’t.
The responders had a few things in common. First, they had more diverse gut bacteria and a larger concentration of a specific type of bacteria called Clostridiales bacteria, specifically in the Ruminococcaceae family. They also had a higher density of one kind of immune cells that fight cancer compared to the 13 who didn’t respond.
Those that did not respond to the treatment, on the other hand, had more of a different type of bacteria in their gut called Bacteroidales.
There’s a good reason why there appears to be a link between the bacteria found in people’s guts and their responses to drugs that act on the immune system, Fred Ramsdell, vice president of research at the Parker Cancer Institute, told Business Insider. The Parker Cancer Institute funded the study, along with the Melanoma Research Alliance and MD Anderson’s Moon Shot program.
Your immune system is fed by the kind of microbes you encounter in your life. Say you have come across a bunch of bacteria in your life, you might have a more robust immune response to a new germ than someone who has come across fewer. It goes along with the “hygiene hypothesis,” the idea that exposure to infections earlier in life could prime the immune system for the future. How exactly this works is still unclear, however. “We the community are still sorting it out,” Ramsdell said.
What to make of the results
The next step is to design a clinical trial targeting the microbiome. That trial, which would be the first of its kind in humans, is expected to launch sometime later this year. Its findings will help show whether there’s a causal relationship between the two, rather than just an association. That could mean giving people a bacterial cocktail (think: some kind of yogurt-like substance), a fecal transplant, or potentially making changes to the diet that could cultivate the ideal kind of bacteria.
But, because there is still a lot researchers need to figure out, it wouldn’t be a good idea — and could even be harmful — to start doing these interventions on your own.
“The best way for people to understand is in the context of a clinical trial,” Dr. Jennifer Wargo, senior author of the study and professor of genomic medicine and surgical oncology at MD Anderson, told Business Insider.
Plus, the observations the researchers were able to make are still too general to leap to any conclusions. “It’s almost certainly more complex,” Ramsdell said. Other factors could influence how people respond too, so even if targeting the microbiome did help some, others still might not benefit from the cancer immunotherapy.
Even so, Wargo considers the results a “paradigm shifter,” when it comes to considering new approaches to get people to respond to these cancer immunotherapy drugs.
SEE ALSO:One of the next epidemic-level chronic diseases doesn’t have any approved treatments — and it could ‘swamp the system’
DON’T MISS:Trump is promising big changes at the FDA — here’s how drugs are approved today
NOW WATCH: The US government just sank a giant ship on purpose — and the footage is amazing