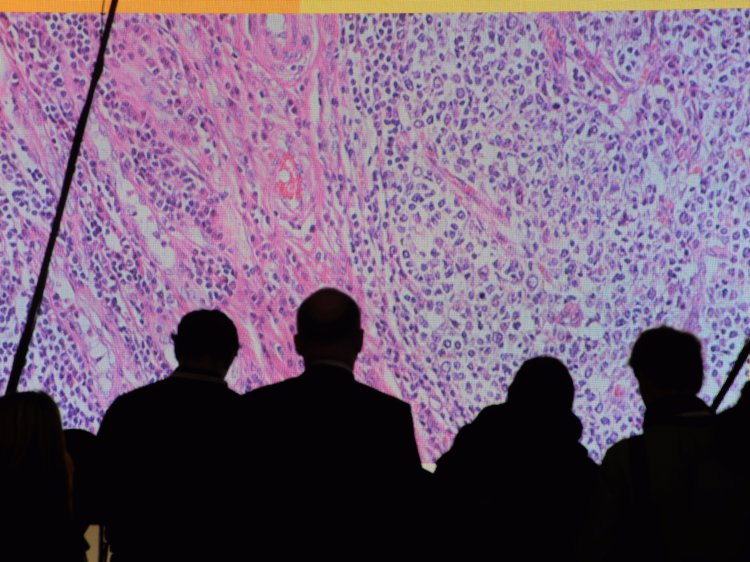
- On Monday, three big players in the growing field of cancer immunotherapy are sharing data that could change how we treat lung cancer.
- The three companies, Bristol-Myers Squibb, Merck, and Roche, are looking at how their immunotherapies, known as checkpoint inhibitors, can be used in combination — either with other immunotherapy or with chemotherapy to treat advanced non-small cell lung cancer.
- Here’s what to expect when the data comes out Monday morning at the American Association of Cancer Research’s annual meeting.
Three pharmaceutical companies are about to release data that could change how we treat lung cancer.
Bristol-Myers Squibb, Merck, and Roche, are looking at how their drugs can be used to treat advanced non-small cell lung cancer. These treatments are part of a new field of cancer treatment called cancer immunotherapy, in which the body’s immune system is manipulated to go after cancer cells.
The trials focus on how effective combinations that leverage certain immunotherapies known as checkpoint inhibitors can be in treating it. According to the American Cancer Society, there are about 234,000 new cases of lung cancer each year. Around 80% to 85% of those cases are a type of lung cancer called non-small cell lung cancer. Overall, lung cancer is the second-most common cancer next to breast cancer in women and prostate cancer in men.
The data will be presented Monday morning at the American Association of Cancer Research’s annual meeting.
The goal will be to show that these treatments can increase the overall survival in patients with advanced lung cancer before it’s treated with anything else. If that’s the case, it could change the way cancer doctors across the US treat lung cancer.
“It’s providing a lot more hope and options for patients of getting better survival benefits when they’re diagnosed with this very serious disease that impacts so many people,” Jill O’Donnell Tormey, CEO of the Cancer Research Institute, which has been exploring cancer immunotherapy for decades, told Business Insider.
Here’s what we know so far about the data that’s coming out on Monday at AACR
- Bristol-Myers Squibb, Checkmate 227: In February, the company showed how its combination of its immunotherapy drugs — Opdivo and Yervoy — managed to work better at keeping cancer patients’ disease from progressing than chemotherapy — that is, in a certain group of lung cancer patients. It’s the only company coming out with a strictly immunotherapy-based regimen compared to chemotherapy. Merck and Roche both have data regarding using their drugs in combination with chemotherapy. BMS’s trial is also unique in that it looks at a new biomarker called tumor mutation burden. The idea is that the more mutations a tumor has, the more likely the immune system will be able to recognize it and go after it. In lung cancer patients who had high TMB (45% of the patients in the trial qualified), the treatment was considered superior to chemotherapy in keeping cancer from progressing.
- Merck, Keynote-189: In January, Merck said its trial combining Keytruda with chemotherapy (pemetrexed and platinum) led to “significantly longer” overall survival and progression-free survival in patients with advanced or metastatic nonsquamous non-small cell lung cancer compared to the chemotherapy alone. Merck already got FDA approval in May 2017 to treat lung cancer using Keytruda and chemotherapy based on data from a phase 2 study.
- Roche, Impower 150: Roche will be presenting data about its trial, which combines the company’s cancer immunotherapy Tecentriq with one of its cancer drugs, Avastin, along with carboplatin and paclitaxel. In March, Roche said the combination helped people with advanced non-squamous non-small cell lung cancer “live significantly longer” than those who received Avastin, carboplatin and paclitaxel alone.
On Monday, we’ll get a better picture of what that means as far as how much longer patients were able to live (known as overall survival), as well as how long they were able to go on the treatment before their cancer started to get worse (something known as progression-free survival).
We’ll also get a sense of something known as the “hazard ratio.” The hazard ratio stacks survival of patients on one arm of the trial compared to the other. So if the ratio is less than one, it means that the immunotherapy-based regimen had better survival than the chemotherapy-only arm.
Already though, the summaries of the results has O’Donnell Tormey optimistic about what it’ll mean for lung cancer patients.
“I guess people are going to have options,” she said.
And ideally that will spread out beyond just academic medical centers to hospitals across the country that see the majority of patients.
“To me, that’s going to be the true game changer for patients,” O’Donnell Tormey said.